Unsafe health care facilities
The problem
One of the most important environments to support the well-being of a child is the clinic or hospital where they receive health care. Yet, thousands of health care facilities are poorly equipped, impacting the delivery of pediatric care for millions of children around the world.
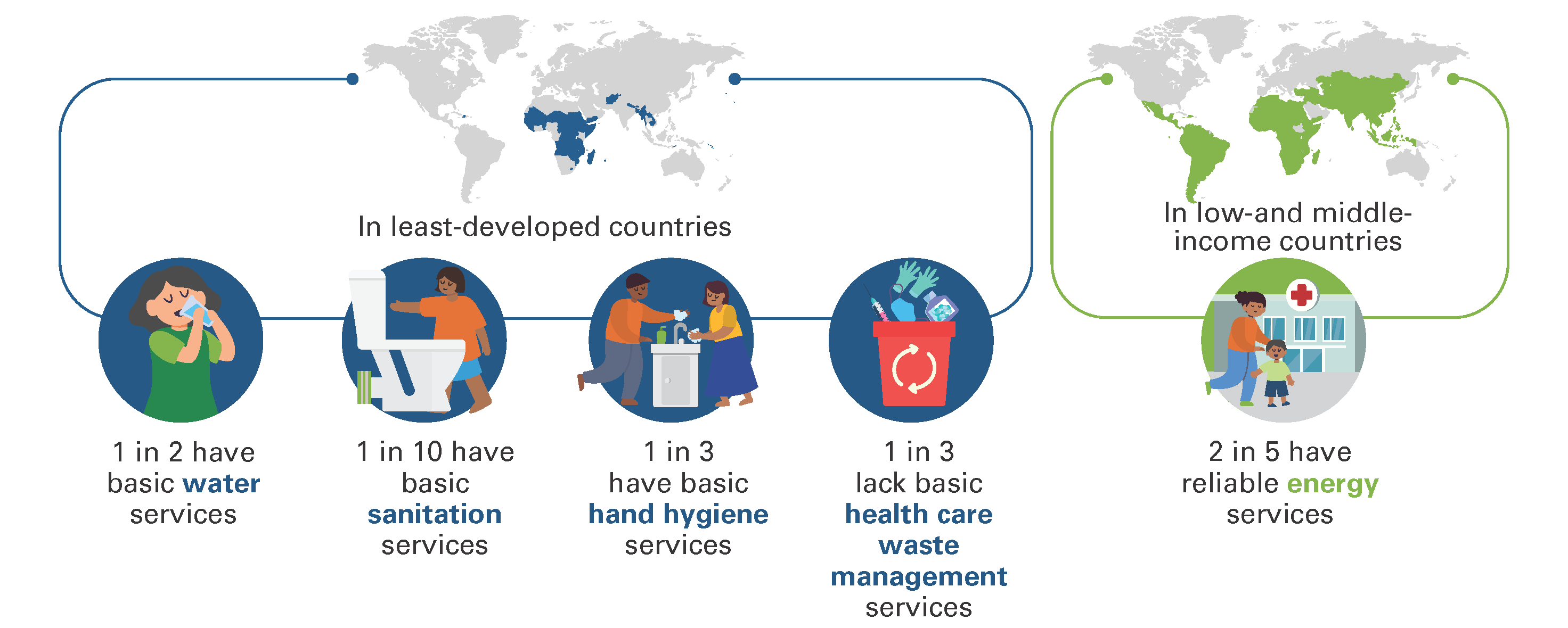
Globally, 1 in 5 health care facilities lack basic water services, 1 in 10 have no sanitation services and 1 in 3 health care facilities lack basic hand hygiene services. Rural, primary health care facilities have the greatest need for improvement. Meanwhile, electricity access in healthcare facilities is also unreliable: more than 1 billion people are served by health care facilities with unreliable electricity or no electricity access at all.
The consequences of poorly equipped health care facilities are significant. Primary health care services necessary for child health, such as labour and delivery, pre- and postnatal care and vaccinations, are contingent upon the availability of appropriate physical infrastructure of the health facility. The lack of water, sanitation and hygiene (WASH), waste and electricity services is an important contributor to poor-quality care, affecting infections, the spread of antimicrobial resistance, uptake of services, staff performance and the dignity of health care facility users.
Health care providers working in facilities with poor infrastructure are facing another threat: climate change. To deliver life-saving health care services without disruption, it is necessary that facility infrastructure is built to withstand these stresses. Yet, the majority of health care facilities and their staff are currently unprepared for such an occurrence.
1
billion
people visit health care facilities without reliable electricity, water, sanitation or waste disposal services.
Thousands of health care facilities lack adequate infrastructure to provide quality care
Areas for intervention

During childbirth, hygiene – and WASH services more generally – have critical impacts on the health outcomes of mothers and babies. Fully functioning WASH services are a crucial aspect of preventing infections, reducing antimicrobial resistance, ending preventable maternal and newborn deaths and responding to outbreaks and emergencies. Approximately 43 per cent of newborn deaths occurred in sub-Saharan Africa, where only half of health care facilities have a water source onsite. Poor WASH services in health care facilities have also been demonstrated to reduce care-seeking behaviours of mothers.
Access to reliable electricity is required for operation and use of a wide variety of vital medical equipment and appliances. In addition, facilities need electricity for adequate lighting systems, refrigeration, cold rooms and IT networks for efficient stock and management of information. When health-care facilities have sufficient and reliable electricity, women can more safely give birth at night and during emergencies, medical equipment can be powered and better sterilized, and clinics can safely store life-saving vaccines and medicines for newborns and children.
Health care facilities produce large quantities of hazardous waste, including needles from vaccines and infectious materials, such as personal protective equipment (PPE). The mismanagement of health care waste can contribute to the spread of potentially pathogenic organisms, while the unsafe burning of waste exposes children to dangerous pollutants. Proper management of waste, including treatment and disposal is necessary for the provision of safe care. Meanwhile, preventing and reducing the amount of waste generated is one of the most effective ways to manage and reduce human and environmental impacts.
For health care facilities to operate without disruption, the essential infrastructure, including WASH, waste and energy, must be regularly maintained. This will require facility staff to be trained on operations and maintenance, with emergency protocols in place in the event of extreme weather events and outbreaks. Staff should also be trained on infection prevention and control measures, particularly those behaviours that are impacted by access to WASH, waste and energy services.
What partners can do
Support the new UN Resolution
on WASH, waste and energy in health care facilities.
Implement policies
that strengthen climate-resilient and environmentally sustainable health care facilities, particularly through WASH, waste and energy services.
Ensure adequate budgets and resourcing
for WASH, waste and electricity services for all facilities, including for operation and maintenance.
Develop and support structures
to enable community members to articulate their needs and demands for quality health services, including provision for WASH, waste and electricity services.
Advocate to governments
and key decision-makers to invest in safe and green health care facilities, including access to WASH, waste management and energy.
Support the development, resourcing and implementation
gf realistic, costed national roadmaps in line with broader Sustainable Development Goal (SDG) 3 acceleration and health programme effort.
Encourage health care facility administrators
to prioritize WASH, waste and energy in providing safe, quality care.
Promote the optimal use of resources
to accelerate WASH, waste and energy improvements in health care facilities.
Conduct implementation research
on the sustainability of WASH, waste and energy services in health care facilities, as well as the impact of such services on children’s health.
Support the health sector
in amplifying messages on the importance of WASH, waste and energy services in health care facilities.
Design cost-effective, green technologies
to support WASH, waste, and energy services in resource-limited health care facilities, including the treatment and disposal of medical waste.
Offer service contract agreements
for operations and maintenance of WASH, waste and energy services in health care facilities, including environmental cleaning.